Work out what each one will mean for you financially as well as for your health and wellbeing and get expert independent financial advice. Often what happens is that the amount of medical retirement pay you are owed will be deducted from any disability compensation you are eligible for through the Department of Veterans Affairs VA.

How To Calculate The Value Of A Guard Reserve Retirement Military Guide
For permanent retirement or placement on the TDRL your compensation is based on the higher of two computations.
/understanding-military-retirement-pay-3332633_final-e2d76ea63bda4604973777b1b3d9d9b2.png)
Medical retirement pay and va disability. Veterans on the TDRL receive no less than 50 percent of their retired pay base. Veterans with 20 years of service OR a disability incurred in the line of duty AND a VA disability rating of at least 10 may be eligible to collect both. Concurrent Retirement and Disability Pay CRDP is a program that provides certain military retirees a monthly restoration of some or all of their VA disability offset.
The member may also be eligible to apply for monthly disability compensation from the Veterans Administration VA if the VA determines the disability is service-connected. Medical disability retirement20 years of active service is not required but all who may be eligible for this retirement option must meet a Physical Evaluation Board to determine whether a medical issue qualifies for medical retirement. Early retirement because of illness or disability If youre thinking of retiring because of ill health or a disability take time to consider your options.
If you receive VA compensation for your VA disability military retired pay is reduced by the VA waiver. Your disability rating times your retired pay base or. Retirees with 20 years of service and a service-connected disability rating between 50-90 are eligible for full VA disability benefits and full military retirement pay.
Two and a half times your years of service times your retired pay base. This is called the VA disability offset to military retirement pay. Concurrent Retirement and Disability Pay CRDP Under CRDP retiree veterans with at least twenty years of service who have a service-connected disability rating between 50 and 90 percent are entitled to receive their entire VA disability compensation benefit as well as their entire military retirement payment.
CRDP is a phase in of benefits that gradually restores a retirees VA disability offset. Concurrent Retirement and Disability Pay CRDP also known as Concurrent Receipt allows military retirees to receive both a full military retirement pension and full VA Disability compensation benefits provided they meet eligibility requirements listed below. CRDP restores retired longevity pay that has been waived to receive VA compensation when the rating is greater than 40 and the retiree has a longevity retirement.
In any case Reserve retirement pay does not become effective until the veteran is 60 years old. The VA waiver is where you waive retired pay to receive VA compensation. The reason is because of double-dipping laws that state you cant be paid twice by the government for the same event.
You qualify for Concurrent Retirement and Disability Pay CRDP if you have a 50 or higher rating from the VA and your retirement is one of three types. Essentially veterans who receive pay and VA disability compensation at the same time are typically subject to the governments double-dipping laws. If youre medically retired you can also qualify but only if you qualify for one of the other three retirements.
Military retirees who choose to receive VA disability compensation will have their military retirement pay offset by the amount of compensation they receive from the VA. However those checks from the VA have no affect on your federal employment or your subsequent federal disability retirement payments. Most retirees choose to receive their VA disability compensation because it is tax-free income while their military pension is taxed by the federal government and by most states.
While maybe not a huge amount at once those checks will add up to a significant amount over time. Not all who qualify may have conditions which are permanent. Disability severance pay equals 2 months basic pay for each year of service not to exceed 12 years a maximum of 24 months basic pay.
The law stipulates that benefits cannot be duplicated. Concurrent Retirement and Disability Pay CRDP allows military retirees to receive both military retired pay and Veterans Affairs VA compensation. Regular TERA or 20-year Reservist at retirement age.
CRSC replaces retired longevity pay waived to receive VA compensation for combat related disabilities. You apply for CRSC through your service branch. Temporary Disability Retirement List TDRL If you are put on the TDRL you will get retirement benefits including a monthly stipend plus medical coverage for you and your dependents until medical.
Some may qualify for temporary disability well cover that below. Armed Forces retirees who are medically retired due to a permanent injury or disability are eligible to collect a military pension as well as disability pay from the US. According to VA concurrent retirement and disability pay CRDP is a phase in of benefits that gradually restores a veterans service pay by eliminating the VA Waiver see below.
This was prohibited until the CRDP program began on January 1 2004. The VA awards a disability rating to the knee of 10 and you begin to receive a check.
Prepare for a successful career in medical billing and coding Get the latest updates on changes in the ICD-10 and PPS Understand how the industry is changing and learn how to stay ahead of the curve Learn about flexible employment options in this rapidly growing industry Medical Billing Coding For Dummies 2nd Edition provides aspiring professionals with detailed information and advice on what to expect in a billing and coding career ways to find a training program certification. Click Download or Read Online button to get Medical Coding book now.
Medical Billing And Coding For Dummies By Smiley Karen Amazon Ae
If youre looking to start a career in the popular field of medical billing and coding this handson friendly guide has you covered.
Medical coding for dummies. But more importantly the implementation of the knowledge into actionable processes ensures better revenue and proper maintenance of patient records. This fully updated second edition of Medical Billing Coding For Dummies provides readers with a complete overview of what to expect and how to succeed in a career in medical billing and coding. People who rely on dummies rely on it to learn the critical skills and relevant information necessary for.
The possibilities are almost endless and if you think about your preferences before you search for a job you can narrow down your list of possible employers saving yourself a boatload of time. Dummies helps everyone be more knowledgeable and confident in applying what they know. Whether its to pass that big test qualify for that big promotion or even master that cooking technique.
Medical Billing Coding For Dummies For Dummies CareerEducation. Your complete guide to a career in medical billing and coding updated with the latest changes in the ICD-10 and PPS This fully updated second edition of Medical Billing Coding For Dummies provides readers with a complete overview of what to expect and how to succeed in a career in medical billing and coding. Medical Billing Coding For Dummies gives you practical easytofollow information and advice on what to expect in a billing and coding career ways to find a training program your certification options ways to stay competitive in the field and the laws and other regulations youll encounter in your work.
Find out about the flexible employment options available and how to qualify. Are you seeking a new career in Medical Coding. People who rely on dummies rely on it to learn the critical skills and relevant information necessary for.
With healthcare providers moving more rapidly to electronic record systems data accuracy and efficient data processing is more important than ever. With healthcare providers moving more rapidly to electronic record systems data accuracy and efficient data processing is more important than ever. Your complete guide to a career in medical billing and coding updated with the latest changes in the ICD-10 and PPS.
The service is provided through a patient group direction developed by our Independent Medical Agency who are registered with and regulated by the Care Quality Commission and the Regulation and Quality Improvement Authority this is a means by which our specifically trained pharmacists can legally supply a prescription only medicine where appropriate. Having full knowledge of the oncology coding cheat sheet can greatly improve the billing and oncology coding methods used in a practice. Where Medical Billing and Coding Specialists Work Before you start job-hunting as a medical billing and coding specialist give some thought to what sort of environment you want to work in.
This site is like a library Use search box in the widget to get ebook that you want. Whether its to pass that big test qualify for that big promotion or even master that cooking technique. Your complete guide to a career in medical billing and coding updated with the latest changes in the ICD-10 and PPS.
If the content Medical Coding not Found or Blank you must refresh this page manually or visit our. With healthcare providers moving more rapidly to electronic record systems data accuracy and efficient data processing is more important than. People who rely on dummies rely on it to learn the critical skills and relevant information necessary for.
Dummies helps everyone be more knowledgeable and confident in applying what they know. Dummies has always stood for taking on complex concepts and making them easy to understand. Whether its to pass that big test qualify for that big promotion or even master that cooking technique.
This video explains the basics of medical codingThank you fo. Are you wondering if Medical Coding is for you. Dummies has always stood for taking on complex concepts and making them easy to understand.
Dummies has always stood for taking on complex concepts and making them easy to understand. Kindle Store Select Your Cookie Preferences We use cookies and similar tools to enhance your shopping experience to provide our services understand how customers use our services so we can make improvements and display ads. From finding the right study course and the latest certification requirements to industry standard practices and insider tips for dealing with government agencies and insurance companies Medical Billing Coding For Dummies has you completely covered.
Dummies helps everyone be more knowledgeable and confident in applying what they know. Download Medical Coding PDFePub or read online books in Mobi eBooks. This fully updated second edition of Medical Billing Coding For Dummies provides readers with a complete overview of what to expect and how to succeed in a career in medical billing and coding.
Bachelors of Science Accounting - Brigham Young University. Presented by Evan M. Part of Medical Billing Coding For Dummies Cheat Sheet The world of medical billing and coding is like one big bowl of alphabet soup because using abbreviations and acronyms in medical records saves time.
Medical Billing Coding For Dummies For Dummies CareerEducation eBook. Masters of Business Administration - Broadview University. Chiropractic CPT and ICD-10 Coding for Dummies.
Doctor of Chiropractic Valedictorian - Palmer College of Chiropractic. Medical Billing and Coding For Dummies.
Pre-authorization is the process that occurs when an insurance company refuses to cover a service unless the provider receives permission to offer you this service. What is Pre Authorization.

Eligibility Benefits Verification And Prior Authorization Services
An insurance plan requirement in which the service provider must notify the insurance company in advance about certain medical procedures or services in order for coverage to be considered.

What is pre authorization in medical billing. Pre Authorization and referral authorizationPre-authorization. With regard to sleep apnea treatment this is most likely used when a dentist is recommending oral appliance therapy. The term authorization refers to the process of getting a medical service s authorized from the insurance payer.
It relates not only whether a service of procedure is covered but also to find out whether it is medically necessary. What is a Pre-Authorization. In medical billing pre authorization is a pre-approval before providing medical service.
The term authorization is also referred to as pre-authorization or prior-authorization. Authorization means physician has to obtain permission from insurance company for rendering certain medical services to patient. It is the process of getting a approval from the insurance carrier to treat specific services.
How to Deal with Prior Authorization in Medical Billing as a medical billing specialist working with prior authorization is an essential part of the work. As a medical billing professional dealing with prior authorization is a necessary part of the job. Prior authorization also known as preauthorization is the process of getting an agreement from the payer to cover specific services before the service is performed.
Preauthorization establishes in advance the Medical Necessity or ExperimentalInvestigational nature of certain care and services covered under this Plan. This approval is required for a number of reasons the main one being that the payers want to avoid unnecessary care and costs. A pre-authorization also known as prior authorization is vital to receiving reimbursement for services while also reducing the risk of a patient being stuck with a large unexpected bill.
Prior Authorization or Pre-Authorization is an essential step in the process of getting health insurance to cover certain services. Medical Insurance Companies or Payers refer to a document or PA form that healthcare providers need to fill up specifying the services needed by a client such as ABA Therapy or other procedures that are. Prior authorization is an integral part of medical diagnosis and procedures especially when the claims are to be settled by an insurance company.
In medical billing pre authorization is a pre-approval before providing medical service. An insurance plan requirement in which the service provider must notify the insurance company in advance about certain medical procedures or services in order for coverage to be considered. It ensures that the Preauthorized care and services described below will not be denied on the basis of Medical Necessity or ExperimentalInvestigational.
Authorization in Medical billing. Prior authorization also known as pre-authorization is the method of receiving approval from the payer to provide certain services prior to the performance of the service. It means that a patient needs to seek permission from the medical insurance provider before undergoing specific medical procedure to claim reimbursement of the bills except during emergencies.
A pre-authorization requirement means that the insurance company will not pay for a service unless the provider a physician or hospital usually gets permission to provide the service. Prior Authorization is a term used actively by medical insurance companies. Pre authorization is the process by which most health insurers determine whether or not to cover a medication service or procedure.
It is a legal obligation to ensure that the insurance payer pays for the specific medical service mentioned in the medical claim form. If authorization has not obtained to treat those healthcare service then claim will be denied not paid from an insurance company. A system whereby a provider must receive approval from a staff member of the health plan such as the health plan Medical Director before a member can receive certain health care services.
Medicare prior Authorization Prior authorization is a process through which a request for provisional affirmation of coverage is submitted to a medical review contractor for review before the item or service is furnished to the beneficiary and before the claim is submitted for processing. To put it simply a pre-authorization is basically a signed agreement from the insurance company stating that they agree to pay for a particular service before it is provided to the patient.
People who rely on dummies rely on it to learn the critical skills and relevant information necessary for. Medical Billing Coding For Dummies gives you practical easy-to-follow information and advice on what to expect in a billing and coding career ways to find a training program your certification options ways to stay competitive in the field and the laws and other regulations youll encounter in your work.
Exploring The Fundamentals Of Medical Billing And Coding
Where Medical Billing and Coding Specialists Work Before you start job-hunting as a medical billing and coding specialist give some thought to what sort of environment you want to work in.

Medical billing for dummies. Dummies helps everyone be more knowledgeable and confident in applying what they know. Therefore medical billing is a process that is dependent on medical coding. Whether its to pass that big test qualify for that big promotion or even master that cooking technique.
This fully updated second edition of Medical Billing Coding For Dummies provides readers with a complete overview of what to expect and how to succeed in a career in medical billing and coding. Find out about the flexible employment options available and how to qualify. The charge entry also.
This updated resource includes details on the most current industry changes in ICD-10 10th revision of the International Statistical Classification of Diseases and Related Health Problems and PPS Prospective Payment. The basic steps involved in medical billing are. Your complete guide to a career in medical billing and coding updated with the latest changes in the ICD-10 and PPS.
Medical billing carried out by a medical biller utilises the diagnosis and procedure codes derived from the medical record documentation to assemble all data concerning the medical bill or claim accurately and efficiently. A medical coder or biller would be smart to obtain training in medical transcription. You are the touchpoint for everyone involved in the healthcare experience from the patient and front office staff to providers and payers.
Your complete guide to a career in medical billing and coding updated with the latest changes in the ICD-10 and PPS. This fully updated second edition of Medical Billing Coding For Dummies provides readers with a complete overview of what to expect and how to succeed in a career in medical billing and coding. With healthcare providers moving more rapidly to electronic record systems data accuracy and efficient data processing is more important than ever.
Medical Billing Coding For Dummies gives you practical easytofollow information and advice on what to expect in a billing and coding career ways to find a training program your certification options ways to stay competitive in the field and the laws and other regulations youll encounter in your work. Charge EntryThe medical biller in this step enters the charges for services provided to the patient. A brief description of the medical billing and coding payment process including the reimbursement cycle for a medical claim.
With healthcare providers moving more rapidly to electronic record systems data accuracy and efficient data processing is more important than ever. A medical transcriptionist would be wise to cross train into medical coding or billing. The possibilities are almost endless and if you think about your preferences before you search for a job you can narrow down your list of possible employers saving yourself a boatload of time.
Medical offices need professionally trained billers and coders either in the office or via telecommute to handle records for internal and external accessibility and efficiency. Therefore people new to the medical credentialing process tend to type keywords like medical credentialing for dummies in the search bar of their web browser. A brief introduction and overview of medical billing including the typical tasks and responsibilities of a medical billing specialist.
If youre looking to start a career in the popular field of medical billing and coding this hands-on friendly guide has you covered. Working as a medical biller and coder is a challenging and rewarding job that takes you right into the heart of the medical industry. Medical billers and coders are essential to the efficient processing of data compliance with government regulations and protection of patient privacy as required by the Health Insurance Portability and Accountability Act HIPAA.
In medical billing companies that function as intermediaries who forward claims information from healthcare providers to insurance payers are known as clearinghouses. Medical Billing Coding For Dummies For Dummies CareerEducation. Recession is a smart idea.
The more varied skill sets one has to fall back on the less chance of floundering during an unexpected job loss. However new people stepping into the medical field as part of the hospital administration may not have any knowledge of medical credentialing. Additionally enhancing your skills.
Medical Billing Coding For Dummies gives you everything you need to know to get started in medical billing and coding. The medical biller in this step enters the charges for services provided to the patient. In what is called claims scrubbing clearinghouses check the claim for errors and verify that it is compatible with the payer software.
From finding the right study course and the latest certification requirements to industry standard practices and insider tips for dealing with government agencies and insurance companies Medical Billing Coding For Dummies has you completely covered. Dummies has always stood for taking on complex concepts and making them easy to understand. Includes a simplified diagram of.
If youre looking to start a career in the popular field of medical billing and coding this handson friendly guide has you covered.
Today process trillions of transactions each year. In what is called claims scrubbing clearinghouses check the claim for errors and verify that it is compatible with the payer software.
In medical billing companies that function as intermediaries who forward medical claims information from healthcare providers to insurance payers are known as clearinghouses.

What is a clearinghouse in medical billing. In what is called claims scrubbing clearinghouses check the claim for errors and verify that it is compatible with the payer software. All in all medical billing clearinghouses are a huge benefit. Criteria for Selecting a Great Medical Billing Clearinghouse.
How to Prevent Medical Billing Claims From Being Denied or Rejected. Clearinghouses are essentially electronic stations or hubs that allow healthcare practices to transmit electronic claims to insurance carriers in a secure way that protects patient health information or protected health information. In medical billing companies that function as intermediaries who forward claims information from healthcare providers to insurance payers are known as clearinghouses.
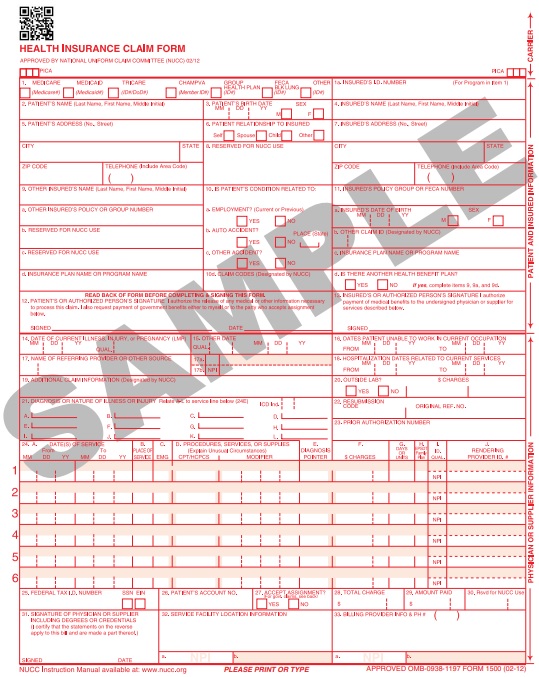
When your practice integrates a clearinghouse into its electronic health record EHR system the clearinghouse reviews any claims and bills you create before those claims or bills get sent to a payer or insurance company. There is also a growing trend towards enhanced patient responsibility both for self-pay and insured patients. The practice management software on a billing professionals computer creates an electronic file the claim also known as the ANSI-X12 837 file.
Additionally clearinghouses offer medical billers and billing. This is what a clearinghouse does in medical billing. An intermediary clearinghouse service provider helps to streamline that process by checking claims for errors storing detailed information on each claim and enabling electronic funds transfer EFT payments.
Clearing house in medical billing is an entity which is used to transmit healthcare claims electronically to the insurance companies for adjudication. Clearing House What is Clearing House. A healthcare clearinghouse is essentially the middleman between the healthcare providers and the insurance payers.
Claims sent electronically are paid much faster than paper claims. What is a Clearinghouse Medical billing clearinghouses take claim information from a billing service or provider check the claims for errors and send this claim information electronically to insurance companies. For example just imagine several million licensed healthcare practitioners each with different medical claim software sending out medical claims to over 5000 different insurance carriers across fifty states each one having its own insurance policies and regulations and then each insurance carrier having their own software program.
Medical billing is often a complicated and time-consuming process. The profitability of physician practices is being squeezed by declining payer reimbursement rates and increasing operating costs. In medical billing companies that function as intermediaries who forward claims information from healthcare providers to insurance payers are known as clearinghouses.
What exactly does a clearinghouse do and why is it important. According to the Department of Health Human Services a health care clearinghouse is a public or private entity including a billing service repricing company or community health information system which processes non-standard data or transactions received from one entity into standard transactions or data elements or vice versa. Whatever the costs are to the medical practice either through individual per claim cost or in software upgrades the benefits are greater.
In laymans terms medical billing clearinghouses are middlemen that take the information found on medical insurance claims and then submits that information electronically to the insurance companies also known as Carriers or Payors that a doctor is contracted with. A medical billing clearinghouse acts as an intermediary that scans claims for common errors standardizes them according to each insurers requirements then submits them to the insurer. The time saved by printing and folding as well as the postage saved mailing the claims is more than the cost of sending the claims.
The medical billing software converts the filed claims into ANSI-X12-837 format to generate an electronic claim The file is then forwarded to the clearinghouse account for claims scrubbingthe process of checking the claim for errors. A clearinghouse checks the medical claims for errors ensuring the claims can get correctly processed by the payer. A medical claims clearinghouse acts as a middleman between the provider doctor dentist chiropractor etc and the payer insurance company.
The Benefits of using a Clearinghouse are. They help to resolve different types of claims in medical billing. What Is a Clearinghouse Rejection.
Lets discuss the role of the medical clearinghouse its benefits and how to choose one. In what is called claims scrubbing clearinghouses check the claim for errors and verify that it is compatible with the payer software. It means clearing house in medical billing acts as an Electronic Data Interchange EDI between healthcare provider and payers.
A medical billing clearinghouse gives you a secondary location from which to manage all your electronic claimsin addition to the backups that you create of your work on a daily basis such as those on your computer on CDDVD tape drives etc.
